Photo by Ashes Sitoula on Unsplash
Early in my career, I used to get frustrated when something in some code stopped a client from doing something better. I learned that, when you are working on a project, you never have the time or the budget to clear all of the hurdles involved in fixing these obstacles. At the time, I worked for a mentor, Mr. Hugh Nash, well known in the engineering world for his commitment to working in the, often tedious, world of codes and standards. Hugh taught me that it was possible, with patience and persistence, to make a difference outside of projects, as well as through use of projects.
Another thing that Hugh taught me was that the codes, as written, tend to result in electrical systems that are significantly larger than the loads they will experience. Now, sizing isn’t just about the loads you measure – there are issues of safety factors and what happens during power outages, and motor starting – but today’s systems are often three and four times larger than the loads they are serving.
In recent years, healthcare organizations have begun to employ LEAN techniques. LEAN is a process derived from Toyota and the Japanese, focused on improving value by removing waste. That philosophy, it seems to me, is highly appropriate to thinking about how we size healthcare electrical systems. It seems to me that, in an era where we are concerned about rising healthcare costs, anything we can do to eliminate waste is something we should pay attention to.
Moreover, eliminating waste is a huge opportunity for sustainability. If we can reduce the size of our electrical systems, without changing needed functionality, we will reduce the amounts of copper and other metals we need; we will improve the efficiency of equipment that does not run well when lightly loaded; we will reduce the amount of stuff that must ultimately end up in landfills.
I spent much of the last two weeks in various meetings with other volunteers, thinking through modifications to the National Electrical Code. I sit as an alternate on the group called Code Making Panel 15 (CMP 15), which has jurisdiction over healthcare facilities, but I also represented a team of volunteer engineers from my company and from around the country, who are conducting research to eliminate some of this waste.
Changing codes can be a tedious, often frustrating process. Changes are often incremental. But over time, the aggregate of incremental changes makes a difference. We’ve seen this in new “standards of care” becoming more acceptable, including the use of fuel cells for emergency power generation, right-sizing emergency generator loads, and even displacement ventilation, as evident in the recently opened (Stanford) Lucile Packard’s Children’s hospital, considered to be one of the most sustainable and technologically advanced hospitals in the U.S.
How does this effect you, our clients?
When you work with Mazzetti, you have the opportunity to help us identify inefficiencies inherent in code and thus, opportunities for change. You get to play a critical role in creating that positive change with us…
I encourage you to continue reading to hear more about the specific work of this committee, but more importantly, how you can get involved too…
CMP 15 had spent a lot of time in four work groups over the last several months in 2017, reviewing a large number of public proposals to update this critical code. At the meeting, we reviewed all of the recommendations from the committees and took final action. The NFPA will publish these results for the public to comment on later this spring. In the meantime, I thought I would share a couple of interesting changes.
1. The NEC is going through what they call a “transition” from the old paradigm of referring to healthcare buildings as buildings, towards the NFPA 99 paradigm of thinking about healthcare spaces. That is, in NFPA 99, two cycles ago, we recognized that the lines between kinds of healthcare facilities are getting blurry. Indeed, one thing we talked about many times in those days was “the Cath lab in a shopping center.” The idea was, healthcare is increasingly leaving what we think of as a hospital and migrating into more and more OTHER kinds of buildings. And, in the end, we don’t care if the Cath Lab is in the hospital or in the shopping mall, we want to be sure the staff and patients are supported and protected. So, NFPA 99 sets up the requirements for healthcare spaces, not healthcare buildings. So, the Cath Lab in the shopping center will have the same outlets, grounding, emergency power, etc as the cath lab in the hospital. The challenge is, the NEC still thinks about buildings and the kinds of things that belong in buildings. This transition began with the current (2017) version of the NEC and will continue into the next (2020) version. We worked hard to try to craft language in the NEC to bridge this divide, and I hope we got it right.
2. Two cycles ago (I think), in NFPA 99, we added the provision that healthcare facilities can use fuel cells as their alternate power sources for their essential electrical systems. This was a pretty big change, but one that is sorely needed. In California, for example, we have very stringent air quality restrictions, and our tried and true solution – diesel generators – are quite problematic from this perspective. Fuel cells generally produce much lower emissions of all pollutants, and are, therefore, preferable from a health perspective (and, after all, isn’t that what ‘HEALTH’ care buildings are about??) There is a large and growing fleet of buildings, including high-reliability facilities such as data centers, that have moved to the use of fuel cells in lieu of diesel generators. So, we know they work. I will write another time about the nuances of this issue, but the point of this particular discussion is that, when the NEC imported the Fuel Cell language from NFPA 99 in the current version, it added the requirement for listing. This is a big problem, as neither UL (who sits on CMP 15 with me) nor any other listing agency has any protocol for listing a fuel cell as an emergency source. So, this cycle, we modified the language to remove the requirement for listing and allow field testing of a fuel cell installation in order to ensure proper operation. This change should allow the use of fuel cells in healthcare facilities in most parts of the US, when enacted. I am working with at least one client to implement a demonstration project using this technology in parallel to their existing diesels. I would LOVE to work with additional clients in other locations – let me know if you are interested.
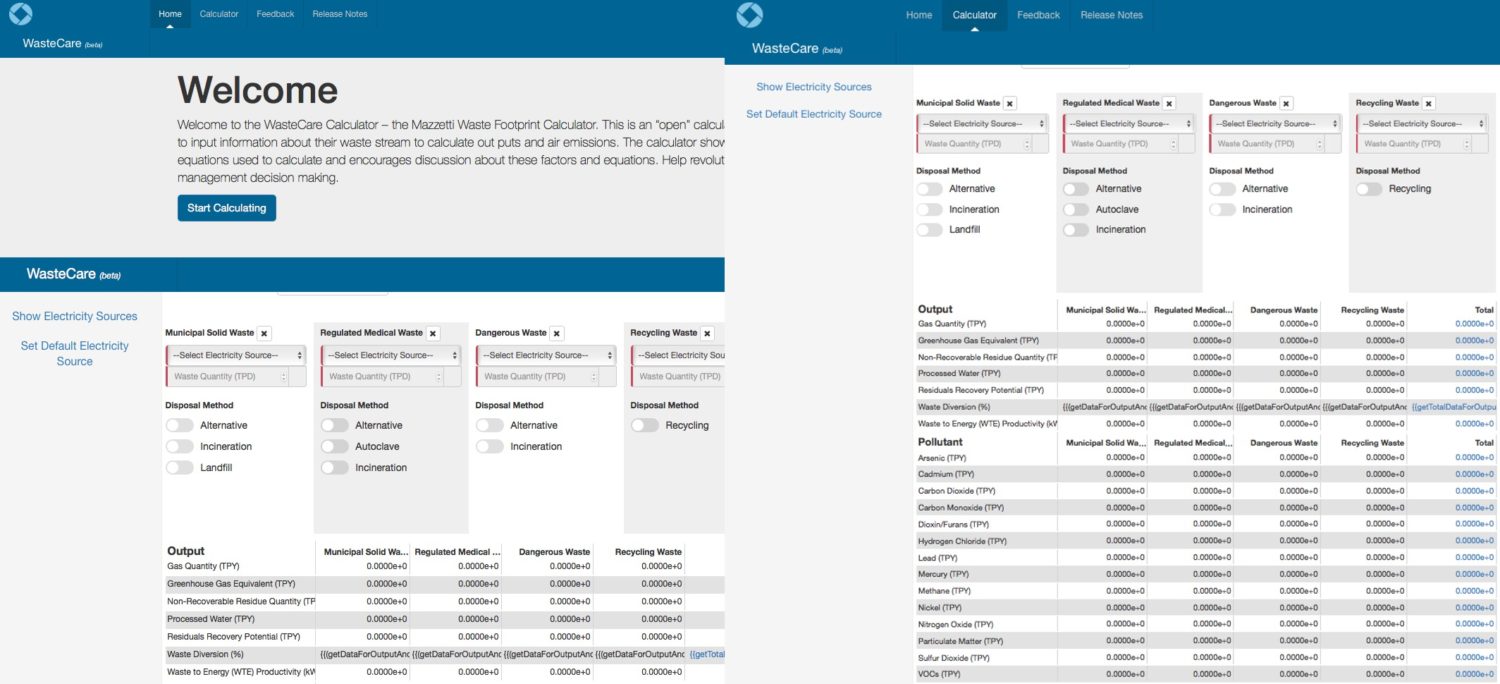
3. Several years ago we performed a research project funded by the California Energy Commission to measure the actual load on branch circuits in medical office buildings. What we found was that our calculations, done in conformance with NEC requirements, significantly overstate the actual demand on most circuits. At a circuit level, this is not so troubling, as we know that someone COULD plug a lot of stuff into one circuit. But, aggregated over an entire department, or floor, or building, these over-sizing factors result in transformers, feeders, switchgear, generators, relative to the actual loads these components will experience during operation. Over the past six months, a collaborative of electrical engineers and hospitals have worked together, with funding from ASHE, to extend this analysis to hospitals. Some of the data is shown in the graph above. This graph shows the connected (red) loads; the NEC calculated load (yellow); the actual load (measured over two weeks – orange); and loads calculated using one of three potential new formulas for sizing these components. In summary, I presented this data to three panels of the NEC: the demand factor committee, the Research Advisory Committee, and the CMP 15 (on which I sit). At this point, “the powers that be” are intrigued, but (understandably) cautious. We created a task force that will work, over the course of 2018, to advance this research and come to consensus on the right way to move forward with appropriate code changes. I will write more on this topic another day, but for now, I am hoping that other engineers and other hospitals will help us. Please let me know!


 Indeed, the energy design of this building was so critical, that in early stages of the project, we worked with the EIR team to craft a Carbon Emissions forecast and a set of sustainability strategies from water to effluent to energy that are remarkable in their aspiration. Many of these ideas originated from the
Indeed, the energy design of this building was so critical, that in early stages of the project, we worked with the EIR team to craft a Carbon Emissions forecast and a set of sustainability strategies from water to effluent to energy that are remarkable in their aspiration. Many of these ideas originated from the 
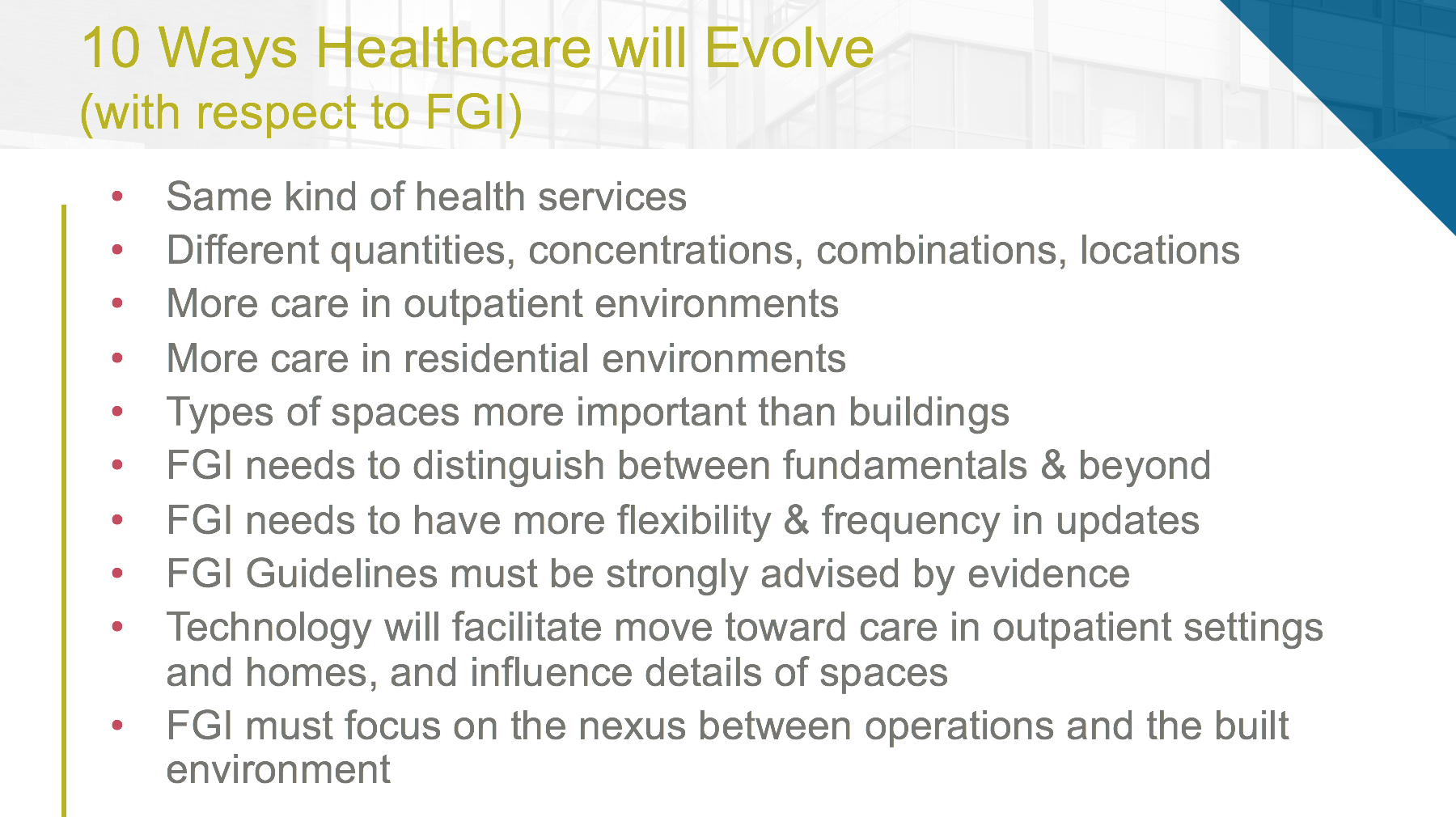 Since that experience, I have been thinking deeply about this–about how the FGI needs to be pursuing its follow-on research to help and how to find ways to help healthcare organizations to respond.
Since that experience, I have been thinking deeply about this–about how the FGI needs to be pursuing its follow-on research to help and how to find ways to help healthcare organizations to respond.