To help further clarify COVID-19 information, we’ve posted some of the fictitious comments we’ve heard and addressed with the corresponding fact. We’ll continue to update. Feel free to send us an email to share additional public health information that may benefit our greater community.
FICTION: The coronavirus disease is smaller than 0.3 micron, so HEPA filters won’t be very effective.
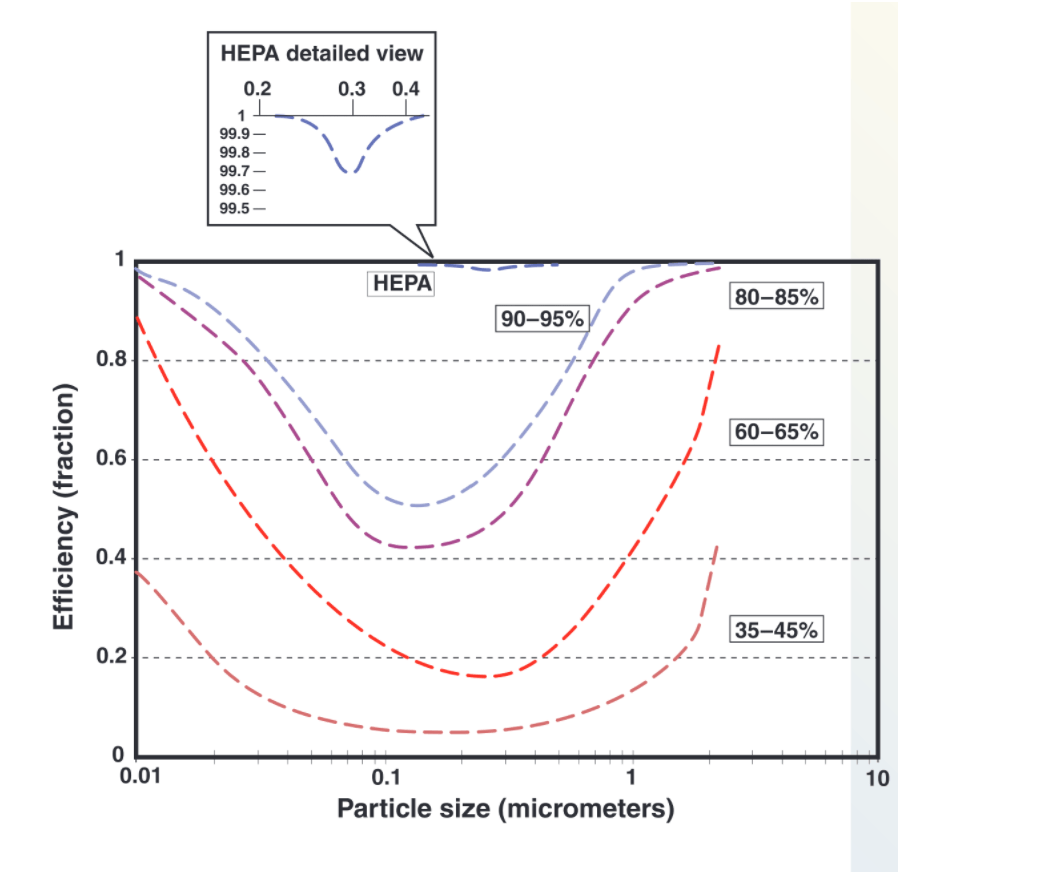
FACT: HEPA filters are rated at 0.3 micron particles because that’s where they are efficient. They are actually more effective with particles both larger and smaller. For the purpose of stopping virus, HEPA filters rated 99.97% or better can be considered effectively absolute filters. If properly installed in a sealed frame system, HEPA-filtered air is safe to return to occupied space. For those who want a deep dive into air filtration, here’s a guidance paper from DHHS/CDC/NIOSH.
FICTION: We probably don’t need HEPA filters, because the filters in my air unit are 90-95% efficient.
FACT: The standard filters required in healthcare facilities are MERV-14. They are rated differently from HEPA filters, so the efficiency ratings should not be compared. Typical viral particles range from about 0.01 to 0.1 micron. While MERV-14 filters are not specifically rated for virus-size particles, the literature suggests that they are roughly 50-60% efficient on virus-size particles. That does provide some dilution, but is not nearly as effective as HEPA filtration. Here’s a figure from the DHHS/CDC/NIOSH paper:
FICTION: Negative pressure protects healthcare personnel from the coronavirus.
FACT: Negative pressure does NOT protect anyone who is in the room with an infected patient. Negative pressure is a containment measure – it may help prevent the spread of the virus from one room to another. PPE is the primary protection measure for persons in the room with an infected patient.
FICTION: I need to use hot water when washing my hands in order to effectively remove any pathogens.
FACT: Temperature is not important for effective hand washing – soap, time, and technique (friction helps remove germs) are what’s important. Washing your hands in cool water will help you retain your natural skin oils while washing often in hot water can cause dermatitis, which can result in your skin harboring more pathogens than normal. (Reference here)
FICTION: If I don’t have COVID-19 symptoms, I am not contagious.
FACT: It takes between 2-10 days (on average 5) for people who are infected with the coronavirus disease to become sick and develop a fever. While people may be most contagious when they are symptomatic, spreading the virus may be possible prior to becoming symptomatic and there have been reports of this occurring with COVID-19. The current recommendation for communities affected by the virus is to practice social distancing and to stay home. Putting distance between yourself and others is a way to protect the whole community and slow the spread of the coronavirus. (Reference here.)
FICTION: There are no resources to evaluate and optimize the shortage of Personal Protective Equipment (PPE) in a facility.
FACT: The “PPE Burn Rate Calculator” is a spread-sheet based interactive tool provided by the CDC that can provide valuable information to help healthcare facilities strategize and optimize the use of PPE during the COVID-19 pandemic. Inventory data is entered by the facility and the model calculates the “burn rate” or average consumption for each category of PPE, allowing the facility to estimate their remaining supply. The tool can be downloaded here.
FICTION: The COVID-19 pandemic is unpredictable and therefore facilities can’t adequately prepare for community spread of the virus.
FACT: This pandemic is unpredictable and unprecedented in modern history, however, healthcare facilities can and should be preparing for a surge in patients requiring care and closely following local and state public health recommendations, as well as the Centers for Disease Control. Actions to prepare for COVID-19 spread in the community include: educating staff on COVID-19, explore the use of telehealth and develop protocols for triaging/assessing patients remotely, determine algorithms to help identify the appropriate level of care for patients (isolate at home vs. emergency care), prepare a safe and efficient triage system to deploy at your facility for patients with respiratory illness, evaluate and optimize use of PPE, and procure additional PPE, if needed. For additional information, review the Interim Guidance for Healthcare Facilities: Preparing for Community Transmission of COVID-19 in the United States on the CDC website.
FICTION: Placing a “negative pressure machine” in the patient room makes it an isolation room.
FACT: What is commonly referred to as a “negative pressure machine” is a portable system that pulls room air through a HEPA filter and blows it back out. If the discharge of the machine is ducted to the outdoors, it may well make the room negative. But, if the machine discharges inside the room, it does not. HEPA filter units can be used to increase room air changes and dilute the number of viral particles that may be suspended in the air. Consulting with a ventilation engineer is a good safeguard.
